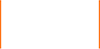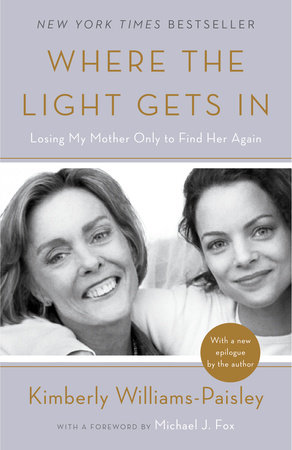

Where the Light Gets In
By Kimberly Williams-Paisley
Foreword by Michael J. Fox
By Kimberly Williams-Paisley
Foreword by Michael J. Fox
By Kimberly Williams-Paisley
Foreword by Michael J. Fox
By Kimberly Williams-Paisley
Foreword by Michael J. Fox
Category: Wellness | Arts & Entertainment Biographies & Memoirs
Category: Wellness | Arts & Entertainment Biographies & Memoirs
-
$17.00
Apr 11, 2017 | ISBN 9781101902974
-
Apr 05, 2016 | ISBN 9781101902967
YOU MAY ALSO LIKE
Mosaic

Let’s Just Say It Wasn’t Pretty
The Prediabetes Diet Plan
Healing and Hope
I Would Find a Girl Walking
Goldie
When God Talks Back
Under Magnolia
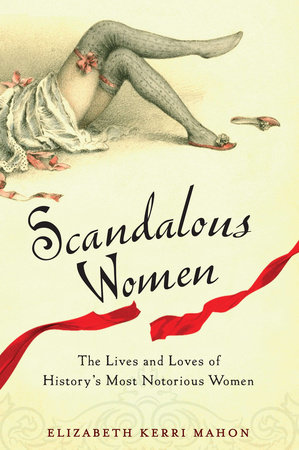
Scandalous Women
Praise
“Heartbreaking but never sentimental, Williams-Paisley’s book offers an intimate look at a family’s struggle with a life-altering disease. It is also a daughter’s tribute to the mother whose disease offered her a new opportunity to ‘love unconditionally…and practice being comfortable with…[the] uncomfortable.’ A simply told, moving memoir.”
—Kirkus Reviews
“Kimberly Williams-Paisley has written a book that is both heartbreaking and essential. I loved it for all the love it contained but also for the wealth of practical information. The Williams family went down a hard road with dementia, and we can all benefit from their experience.”
—Ann Patchett, New York Times bestselling author of Bel Canto and State of Wonder
“The relationship between a mother and daughter is one of the most complicated and meaningful there is. Kimberly Williams-Paisley writes about her own with grace, truth, and beauty as she shares her journey back to her mother in the wake of a devastating illness.”
—Brooke Shields, New York Times bestselling author of There Was a Little Girl
“Kim’s story really resonated with me, as it will with countless others. Her beautiful, heartfelt book is an absolute must-read for mothers, daughters, and anyone dealing with a loved one living with dementia. It will also help to bring comfort to families facing any type of life-altering situation.”
—Robin Roberts, Good Morning America
“Where the Light Gets In is simply wonderful . . . and sad . . . and brave. This book will bring comfort to families who are experiencing the complex and confusing journey of progressive dementia while still celebrating moments of true joy. Williams-Paisley’s narrative and the resource section will help people know they are not alone.”
—Angela Timashenka Geiger, Chief Strategy Officer, Alzheimer’s Assocation
“Generous, human, and healing; that’s what this book is. Kimberly Williams-Paisley has invited us into her life and her family so that we may know ourselves better. By sharing her story with such vulnerability and honesty, she makes it accessible to everyone, with or without a personal connection to dementia. Through it, I had the experience of seeing my own family differently, understanding my desire to love more, and connecting deeply to my own stories of illness, grief, compassion, empathy, and redemption.”
—Connie Britton, Actress
“Where the Light Gets In left an indelible mark on my heart. The story of love and acceptance and the unbreakable bond of family, this book will be a comfort to so many families who are going through what Kim’s went through and will be a much-needed source of strength for all those who read it.”
—Sheryl Crow, Musician
“Informative, relatable, and heartbreaking, Where the Light Gets In is a must-read for those who have a loved one struggling with dementia.”
—Seth Meyers, Host of Late Night with Seth Meyers
“Kimberly Williams-Paisley’s experience with her mother’s dementia is very moving, and you’ll be touched by so much in this book. This topic needs national attention, and Where the Light Gets Inhelps bring focus to that need.”
—William Shatner, Actor
“In Where the Light Gets In, Kimberly Williams-Paisley shares the brutal emotional toll that dementia takes on a family, bravely revealing the denial, the missteps, the losses, the grief. Thankfully, she also shares the lessons–how to get comfortable being uncomfortable, how to connect with her mother where she is, how to love unconditionally. Intimate, honest, and beautifully written, this book will be a tremendous resource for anyone affected by dementia.”
—Lisa Genova, New York Times bestselling author of Still Alice
“Kimberly Williams-Paisley’s honest and heart-wrenching memoir draws a stark picture of the devastation of dementia on a family and captures the sense of injustice when the parent/child role is reversed far too young. Kimberly shares her story to honor her mother, but she galvanizes us to find a cure for a disease that slowly erases the ones we love most.”
—Lee Woodruff, journalist and New York Times bestselling coauthor of In An Instant
21 Books You’ve Been Meaning to Read
Just for joining you’ll get personalized recommendations on your dashboard daily and features only for members.
Find Out More Join Now Sign In